- Home
- About
- Facility
- Telemedicine
-
Surgeries
- Cervical (Neck)
- Thoracic (Upper Back)
- Lumbar (Lower Back)
-
Minimally Invasive
- Advanced Spine Surgery
- Alternatives to Disc Replacement
- Alternatives to Spinal Fusion
- Back Stimulator Implant
- Bulging Disc Surgery
- Cervical Artificial Disc Surgery
- Cervical Discectomy
- Cervical Facet Joint Surgery
- Cervical Microdiscectomy
- Discectomy
- Disc Herniation Surgery Los Angeles
- Endoscopic Discectomy
- Foraminotomy
- Implanted Spinal Cord Stimulator
- Interspinous Devices
- Interspinous Spacers
- Laminectomy
- Laser discectomy
- Laser Spine Discectomy
- Laser Spine Surgery
- Minimally Invasive Decompression
- Minimally Invasive Herniated Disc Surgery
- Minimally Invasive Neck Surgery
- Minimally Invasive Spine Surgery
- Orthopaedic Spine Surgery
- Percutaneous Discectomy
- Percutaneous Lumbar Discectomy
- Rhizotomy
- Rhizotomy Procedure
- Rhizotomy Surgery
- Sciatica Surgery
- Spinal Cord Stimulation
- Spinal Cord Stimulator Implant
- Spinal Sparcers
- Spinal Spacers for Stenosis
- Spinal Surgery
- Sacroiliac (Pelvic)
- Programs
- FAQ
- Patient Education
- Q&A
- Contact
- Reviews
- Home
- About
- Facility
- Telemedicine
-
Surgeries
- Cervical (Neck)
- Thoracic (Upper Back)
- Lumbar (Lower Back)
-
Minimally Invasive
- Advanced Spine Surgery
- Alternatives to Disc Replacement
- Alternatives to Spinal Fusion
- Back Stimulator Implant
- Bulging Disc Surgery
- Cervical Artificial Disc Surgery
- Cervical Discectomy
- Cervical Facet Joint Surgery
- Cervical Microdiscectomy
- Discectomy
- Disc Herniation Surgery Los Angeles
- Endoscopic Discectomy
- Foraminotomy
- Implanted Spinal Cord Stimulator
- Interspinous Devices
- Interspinous Spacers
- Laminectomy
- Laser discectomy
- Laser Spine Discectomy
- Laser Spine Surgery
- Minimally Invasive Decompression
- Minimally Invasive Herniated Disc Surgery
- Minimally Invasive Neck Surgery
- Minimally Invasive Spine Surgery
- Orthopaedic Spine Surgery
- Percutaneous Discectomy
- Percutaneous Lumbar Discectomy
- Rhizotomy
- Rhizotomy Procedure
- Rhizotomy Surgery
- Sciatica Surgery
- Spinal Cord Stimulation
- Spinal Cord Stimulator Implant
- Spinal Sparcers
- Spinal Spacers for Stenosis
- Spinal Surgery
- Sacroiliac (Pelvic)
- Programs
- FAQ
- Patient Education
- Q&A
- Contact
- Reviews
Endoscopic transforaminal lumbar discectomy
What is endoscopic transforaminal lumbar discectomy used for?
Endoscopic transforaminal lumbar discectomy is a minimally invasive procedure that is used for the treatment of painful disc herniations in the low back or lumbar spine. There are 5 lumbar vertebral segments. Each segment consists of a disc attached to the vertebra above and below that disc. The disc is attached to the vertebra via the annulus fibrosis, a fibrous band. This fibrous band holds in place the soft disc nucleus.
With repetitive use or with sudden injury, the annulus fibrosis of the disc might tear. The tear may be partial or may extend all the way through the disc and into the central spinal canal. In a disc herniation, the disc tear results in displacement of the soft disc nucleus through the tear in the annulus. The disc may extend partially through the tear or may extend all the way through, into the spinal canal.
Disc herniations can cause pain or dysfunction through several mechanisms. Commonly, the disc tear itself may be painful. In addition to pain from the disc, the disc material extending through the tear can compress the nerve sac traveling through the spinal canal. This can result in radiculopathy leading to limb pain, numbness, tingling or weakness. If severe enough, this compression can result in balance problems and bowel and bladder incontinence.
How is an endoscopic transforaminal lumbar discectomy performed?
Endoscopic transforaminal lumbar discectomy is performed utilizing an endoscope. An endoscope is a small tube inserted into the body, allowing the surgeon to look inside the spine. Because the endoscope is small, only a small band-aid like incision is required. The endoscope has a precision lens on one end and a high definition (HD) camera on the other end. Microscopic instruments are passed through the endoscope to perform surgery. The surgeon visualizes the entire operation, from inside the spine, using the endoscope mounted HD camera. The surgical video is projected on a high-resolution monitor or heads up display.
To start the procedure, a small incision is made on the skin at the lower back, about 10cm from the middle of the back and near the flank. A small tube about 7mm in diameter, (less than half the size of a dime), is then placed through the small incision and through a natural opening in the spine, the foramen. A small endoscope is placed through the 7mm tube. Specialized micro-instruments are then used to remove the torn and herniated disc and relieve pressure on adjacent nerves. Surgery is guided by real time HD video and x-rays.
What are the advantages of endoscopic transforaminal lumbar discectomy?
Endoscopic transforaminal lumbar discectomy allows the surgeon to remove the herniated and protruding portion of a low back or lumbar disc that is causing low back pain or sciatica. Unlike traditional surgery, this is done by accessing the spine through a natural opening where nerves leave the spine. This opening is called the foramen. By performing surgery through the small foramen, endoscopic transforaminal lumbar discectomy can spare the normal spinal structures that are typically injured at surgery. Many of these structures are important components to spinal strength and stability. These include the muscles at the back of the spine, the lumbar facet joint and the ligamentum flavum, the most elastic ligament in the spine.
Sparing normal spinal structures from surgical damage means that patients can recover more quickly and get back to their previous status faster. Patients can perform light activity and exercise after a day or so. Athletes or those with physical occupations can often return to their activities with little or no rehabilitation since the muscles, joints and ligaments of the spine remain strong and uninjured.
What are the alternatives to endoscopic transforaminal lumbar discectomy?
Patients with painful lumbar disc herniations resulting in back pain, sciatica or lumbar nerve radiculopathy are usually first treated with injections. The most common procedure is a lumbar epidural steroid injection. In this procedure, a physician uses x-rays to guide a small needle through the natural openings of the spine. An anesthetic and strong anti-inflammatory steroid medication mixture is then injected.
In patients with persistent symptoms after injections or other conservative care, surgery is considered. The most common procedure is a micro-discectomy. In this procedure a small incision is made in the back. A 22 mm tube is inserted through the back muscles and is placed against the bony portion of the vertebra of the affected spinal segment. Using a microscope, the surgeon then drills away the middle portion of the lumbar facet joint and portions of the lamina, or bony ring surrounding the spinal canal. The ligamentum flavum attached to the lamina is also removed. The nerve sac is then retracted before the disc is finally reached. A small incision is made in the disc and the disc herniation is removed.
How long will the procedure take?
The endoscopic transforaminal lumbar discectomy surgery typically takes an hour for each disc treated. You will be in the operating room for an additional hour preparing for surgery and preparing for recovery. After the procedure you will recover for about two hours before going home.
What is the recovery like?
After endoscopic transforaminal lumbar discectomy you will go home the same day with pain medications. In most cases light activity can be resumed the next day. Activity should be tolerably increased over 7 days and should consist of short walks, light exercise and a gradual return to normal daily activities. Avoid strenuous activity and heavy lifting (over 10 to 15 pounds) for the first several weeks. If one’s job is sedentary then work can be resumed in 7 days. Recovery time will vary based on individual factors.
Endoscopic interlaminar lumbar discectomy
What is endoscopic interlaminar lumbar discectomy used for?
Endoscopic interlaminar lumbar discectomy is a minimally invasive procedure that is used for the treatment of painful disc herniations in the low back or lumbar spine. There are 5 lumbar vertebral segments. Each segment consists of a disc attached to the vertebra above and below that disc. The disc is attached to the vertebra via the annulus fibrosis, a fibrous band. This fibrous band holds in place the soft disc nucleus.
With repetitive use or with sudden injury, the annulus fibrosis of the disc might tear. The tear may be partial or may extend all the way through the disc and into the central spinal canal. In a disc herniation, the disc tear results in displacement of the soft disc nucleus through the tear in the annulus. The disc may extend partially through the tear or may extend all the way through, into the spinal canal.
Disc herniations can cause pain or dysfunction through several mechanisms. Commonly, the disc tear itself may be painful. In addition to pain from the disc, the disc material extending through the tear can compress the nerve sac traveling through the spinal canal. This can result in radiculopathy leading to limb pain, numbness, tingling or weakness. If severe enough, this compression can result in balance problems and bowel and bladder incontinence.
The endoscopic interlaminar discectomy procedure is commonly performed at L5/S1 where the bones of the pelvis might preclude an endoscopic transforaminal approach. The procedure is also used to treat large, extruded disc herniations that might not be easily reached via the endoscopic transforaminal approach.
How is an endoscopic interlaminar lumbar discectomy performed?
Endoscopic interlaminar lumbar discectomyis performed utilizing an endoscope. An endoscope is a small tube inserted into the body, allowing the surgeon to look inside the spine. Because the endoscope is small, only a small band-aid like incision is required. The endoscope has a precision lens on one end and a high definition (HD) camera on the other end. Microscopic instruments are passed through the endoscope to perform surgery. The surgeon visualizes the entire operation, from inside the spine, using the endoscope mounted HD camera. The surgical video is projected on a high-resolution monitor or heads up display.
To start the procedure, a small incision is made on the skin at the lower back, near the middle of the back. A small tube about 8mm in diameter, (less than half the size of a dime), is then placed through the small incision and through an opening between the bones of the back of the spine. This opening is called the interlaminar space. A small endoscope is placed through the 8mm tube. Specialized micro-instruments are then used to remove the torn and herniated disc and relieve pressure on adjacent nerves. Surgery is guided by real time HD video and x-rays.
What are the advantages of endoscopic interlaminar lumbar discectomy?
Endoscopic interlaminar lumbar discectomy allows the surgeon to remove the herniated and protruding portion of a low back or lumbar disc that is causing low back pain or sciatica. Like a traditional micro-discectomy, this is done by accessing the spine through a natural opening in the back of the spine, between the vertebrae. Unlike a microdiscectomy, the tools used to accomplish an endoscopic interlaminar lumbar discectomy are small enough that disruption of normal spinal structures is minimized. The endoscopic procedure can be performed with insignificant disruption to the muscles of the back, a tiny (about 8mm) incision through the ligament between the vertebra and usually no trauma at all to the lumbar facet joints.
Sparing normal spinal structures from surgical damage means that patients can recover more quickly and get back to their previous status faster. Patients can perform light activity and exercise after a day or so. Athletes, or those with physical occupations, can often return to their activities with little or no rehabilitation since the muscles, joints and ligaments of the spine remain strong and uninjured.
Another advantage of endoscopic interlaminar lumbar discectomy is that it allows an endoscopic minimally invasive operation in cases where one could not otherwise be performed. In males, the bones of the pelvis often obstruct an endoscopic transforaminal lumbar discectomy approach. By approaching the spine near the middle of the back, the endoscopic interlaminar lumbar discectomy can be facilitated in these cases.
Lastly, some disc herniations are large and protrude well into the spinal canal. Approaching these herniations via an endoscopic transforaminal approach can be difficult. Through the endoscopic interlaminar approach these herniations can be reached directly and such large herniations can be removed from the spine.
What are the alternatives to endoscopic interlaminar lumbar discectomy?
Patients with painful lumbar disc herniations resulting in back pain, sciatica or lumbar nerve radiculopathy are usually first treated with injections. The most common procedure is a lumbar epidural steroid injection. In this procedure, a physician uses x-rays to guide a small needle through the natural openings of the spine. An anesthetic and strong anti-inflammatory steroid medication mixture is then injected.
In patients with persistent symptoms after injections or other conservative care, surgery is considered. The most common procedure is a micro-discectomy. In this procedure a small incision is made in the back. A 22 mm tube is inserted through the back muscles and is placed against the bony portion of the vertebra of the affected spinal segment. Using a microscope, the surgeon then drills away the middle portion of the lumbar facet joint and portions of the lamina, or bony ring surrounding the spinal canal. The ligamentum flavum attached to the lamina is also removed. The nerve sac is then retracted before the disc is finally reached. A small incision is made in the disc and the disc herniation is removed.
How long will the procedure take?
The endoscopic interlaminar lumbar discectomy surgery typically takes an hour for each disc treated. You will be in the operating room for an additional hour preparing for surgery and preparing for recovery. After the procedure you will recover for about two hours before going home.
What is the recovery like?
After endoscopic interlaminar lumbar discectomy you will walk go home the same day with pain medications. In most cases light activity can be resumed the next day. Activity should be tolerably increased over 7 days and should consist of short walks, light exercise and a gradual return to normal daily activities. Avoid strenuous activity and heavy lifting (over 10 to 15 pounds) for the first several weeks. If one’s job is sedentary then work can be resumed in 7 days. Recovery time will vary based on individual factors.
Endoscopic lumbar decompression
What is endoscopic lumbar decompression utilized for?
Endoscopic lumbar decompression is a minimally invasive procedure that is used for the treatment of lumbar spinal stenosis. Lumbar spinal stenosis is a degenerative condition of the lumbar spine. In lumbar spinal stenosis, repetitive stress of the lumbar spine results in overgrowth, called hypertrophy, of the stabilizing elements of the spine. These elements include the facet joints and the ligamentum flavum. The facet joints are paired joints on either side of the vertebra that join the vertebra with the vertebra above and below. The ligamentum flavum is a ligament which connects the bony spinal ring, called the lamina, to the lamina above and below. The hypertrophy of these elements results in narrowing of the normal spinal nerve passageways. This results in compression of the nerves traveling through these passageways. In addition, degeneration may result in disc bulging. This disc bulging extends into the nerve passageways as well, further worsening the narrowing of the spinal nerve passageways.
Spinal stenosis may result in several symptoms. When spinal stenosis results in compression of the nerves exiting the spine, this results in lumbar radiculopathy. Lumbar radiculopathy is pain, loss of sensation or weakness caused by nerve dysfunction. When spinal stenosis results in compression of the nerve sac traveling through the spine this may result in lumbar radiculopathy, balance problems, or bowel and bladder incontinence.
Since the spinal nerve passageways narrow with an upright or standing posture, standing usually makes symptoms worse. Bending forward or sitting makes symptoms better.
How is Endoscopic lumbar decompression performed?
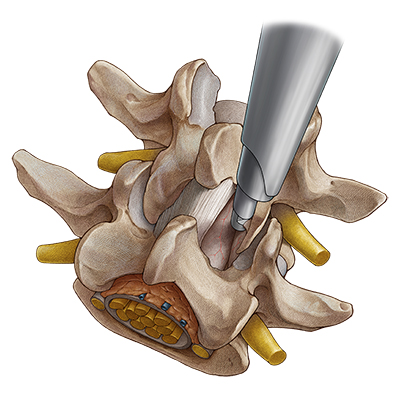
Artist rendering of endoscopic lumbar decompression (courtesy of RIWOspine GmbH).
Endoscopic lumbar decompression is performed utilizing an endoscope. An endoscope is a small tube inserted into the body, allowing the surgeon to look inside the spine. Because the endoscope is small, only a small band-aid like incision is required. The endoscope has a precision lens on one end and a high definition (HD) camera on the other end. Microscopic instruments are passed through the endoscope to perform surgery. The surgeon visualizes the entire operation, from inside the spine, using the endoscope mounted HD camera. The surgical video is projected on a high-resolution monitor or heads up display.
Endoscopic lumbar decompression is a minimally invasive procedure for the treatment of spinal stenosis. Spinal stenosis is a condition that narrows and compresses the normal nerve passageways of the spine. These passageways are found in the spinal canal (the opening in the back of the spine that travels from your head to your tailbone) and the foramen (the opening at each side of the spine that allows nerves to travel out of the spine). Nerve passageways in the spinal canal are narrowed due to degeneration and enlargement of the facet joints (joints on either side of the vertebra) or due to degeneration and enlargement of the ligamentum flavum (the elastic ligament that joins vertebra together in the back of the spine). Nerve passageways in the foramen are narrowed by degeneration and enlargement of the lumbar facet joints or bony spurs arising from the vertebra. Sometimes a bulging disc will also contribute to nerve passageway narrowing in both the spinal canal and foramen.
Posterior decompression is a form of lumbar decompression performed on the back of the spine. When performing endoscopic lumbar decompression from the back of the spine, a small incision is made on the skin at the lower back, near the middle of the back. A small tube 10.5mm in diameter, (slightly more than half the size of a dime), is then placed through the small incision through an opening between the bones of the back of the spine. This opening is called the interlaminar space. A small endoscope is placed through the 10.5mm tube. Specialized micro-instruments are then used to remove overgrown lumbar facet joints, ligament and disc bulges placing pressure on nerves traveling through the spine. Surgery is guided by real time HD video and x-rays.
Transforaminal decompression is a form of lumbar decompression performed from the side. When performing this form of lumbar decompression, a small incision is made on the skin at the lower back, near the flank. A small tube 8mm in diameter, (slightly less than half the size of a dime), is then placed through the small incision and docks at the facet joints narrowing the foramen. Specialized micro-instruments are then used to open the foramen and release pressure on nerves. Surgery is guided by real time HD video and x-rays.
What are the advantages of endoscopic lumbar decompression?
Endoscopic lumbar decompression allows the surgeon to open the narrowed nerve passageways of the spine that are affected by spinal stenosis. Since the ligamentum flavum, facet joints and bulging discs are narrowing nerve passageways in spinal stenosis, these structures must be partially removed to free up the nerves of the spine. Endoscopic lumbar decompression allows partial removal of these structures while minimalizing collateral damage to normal spinal structures.
Posterior decompression is used to treat spinal stenosis in the central and sides of the spinal canal. In these cases, endoscopic lumbar decompression must remove part of the ligamentum flavum and part of the facet joint, just as in conventional laminotomy surgery. However, smaller instruments means that a smaller incision and access tube can be used, minimizing disruption of the multifidus muscle of the back.
Transforaminal decompression is used to treat spinal stenosis in the foramen and one side of the spinal canal. A portion of the facet joint is undercut, enlarging the opening. The multifidus muscle of the back and the ligamentum flavum, a key stabilizing ligament, are left entirely intact. This speeds up recovery and maintains spinal strength and stability.
Another key advantage to transforaminal decompression is that the foramen can be decompressed in its entirety, from the inside. Conventional surgery, on the other hand, has difficulty in reaching this region and it is a common reason for failed surgery.
What are the alternatives to endoscopic lumbar decompression?
The first-line treatment for patients suffering from spinal stenosis is epidural steroid injection. In this procedure, a tiny needle is guided by x-rays into the spinal nerve passageways. A combination of anesthetic medication and a powerful anti-inflammatory steroid medication is injected.
The surgical alternative for the treatment of spinal stenosis is micro-laminotomy. In this procedure, a small incision is made in the back. A 22 mm tube is then advanced through the muscle and docked on the bony elements in the back of the spine. Using a microscope, the surgeon then drills away at the middle of the facet joint and the bony ring of the lamina. The ligamentum flavum is removed. In this fashion, the nerve passageways are decompressed.
Another alternative for the treatment of spinal stenosis is the placement of an interspinous spacer. In this procedure, a metal device is placed between the bones of the back of the vertebra. This device separates the back of the vertebra from one another and enlarges the nerve passageways of the spine.
How long will the procedure take?
The endoscopic lumbar decompression surgery typically takes one to two hours for each spine level treated. You will be in the operating room for an additional hour preparing for surgery and preparing for recovery. After the procedure you will recover for about two hours before going home.
What is the recovery like?
After endoscopic lumbar decompression you will go home the same day with pain medications. In most cases light activity can be resumed the next day. Activity should be tolerably increased over 7 days and should consist of short walks, light exercise and a gradual return to normal daily activities. Avoid strenuous activity and heavy lifting (over 10 to 15 pounds) for the first several weeks. If one’s job is sedentary then work can be resumed in 7 days. Recovery time will vary based on individual factors.
Endoscopic lumbar fusion
What is endoscopic lumbar fusion utilized for?
Endoscopic lumbar fusion is used for the treatment of low back pain due to degenerated disc or instability of the spine. Instability of the spine is the abnormal and painful movement of one vertebra on another. This is sometimes referred to as a “slippage” when one vertebra has slipped forward on another. The medical term for “slippage” is spondylolisthesis.
How is an endoscopic lumbar fusion performed?
Endoscopic lumbar fusion is performed utilizing an endoscope. An endoscope is a small tube inserted into the body, allowing the surgeon to look inside the spine. Because the endoscope is small, only a small band-aid like incision is required for its insertion. The endoscope has a precision lens on one end and a high definition (HD) camera on the other end. Microscopic instruments are passed through the endoscope to perform surgery. The surgeon visualizes the entire operation, from inside the spine, using the endoscope mounted HD camera. The surgical video is projected on a high-resolution monitor or heads up display.
To start the procedure, a small incision is made on the skin at the lower back, near the flank. A small tube about 8mm in diameter, (less than half the size of a dime), is then placed through the small incision and through the foramen of the spine, a natural opening where nerves exit the sine. A small endoscope is placed through the 8mm tube. Surgery is guided by real time HD video and x-rays. Using specialized micro-instruments, the foramen can be enlarged to facilitate the fusion surgery. Through the endoscope, passing across the foramen, the disc is removed. After removing the disc, a polymer and/or metal implant is placed between the vertebrae. A mixture of bone and bone marrow is injected into the space, around the implant.
Over time, a solid bridge of bone will form between the vertebrae. This is called a fusion. It takes about a year for fusion to fully occur. To provide stability during that time, screws will be inserted in the back of the vertebra to join adjacent vertebra that have undergone the fusion procedure.
What are the advantages of endoscopic lumbar fusion?
Fusion procedures are by nature more invasive than other spinal operations. Endoscopic lumbar fusion makes a fusion as minimally invasive as possible. Conventional fusion procedures are performed from the back of the spine. This results in disruption of the multifidus muscle, removal of part of the facet joint and removal of the ligamentum flavum. These are key stabilizing structures of the spine. Endoscopic lumbar fusion allows the fusion procedure to be done through a natural opening in the spine, the intervertebral foramen. This prevents disruption to the stabilizing structures in the back of the spine, allowing a more stabilized and stronger spine after the fusion procedure.
What are the alternatives to endoscopic lumbar fusion?
There are different techniques and approaches to performing a lumbar fusion. Surgery can be performed directly from the back, slightly off to the side of the spine, from the side of the spine or from in front of the spine. Whatever the approach, these different techniques all involve removal of the disc and placement of bone graft in the disc space.
In many instances, the same benefits of fusion can be conferred through non-fusion endoscopic surgery. Endoscopic discectomy can often successfully address pain arising from the spinal disc. Additionally, when pain arises from the joints of the spine, endoscopic rhizotomy can provide pain relief. However, when pain arises form abnormal motion of the spine, (a slippage of one vertebra on another with normal movements), fusion is often the best surgical answer.
How long will the procedure take?
The endoscopic lumbar fusion surgery takes one and a half to two hours. You will be in the operating room for an additional hour preparing for surgery and preparing for recovery. After the procedure you will recover for two to four hours before going home.
What is the recovery like?
After surgery, you will go home the same day with pain medications. For the first several days we advise plenty of rest with light stretching. In the first week exercise is limited to short walks. Avoid heavy lifting (greater than 10 to 15 pounds), bending or twisting for the first several months. You can return to work at 4 weeks unless work requires strenuous activity. At 4 weeks a progressive physical therapy program can be started. While minimally invasive surgery allows a faster recovery and easier rehabilitation, individual factors will dictate recovery time.
Endoscopic lumbar extra-dural nerve avulsion (EDNA) or endoscopic lumbar rhizotomy
What is endoscopic lumbar EDNA (or rhizotomy) used for?
Endoscopic lumbar EDNA (or rhizotomy) is a minimally invasive procedure that is used for the treatment of low back pain due to an injured or painful lumbar facet joint. The lumbar facet joint is a paired joint, just behind and on either side of the disc.
Lumbar facet pain may be caused by wear and tear of the facet joint. This is usually seen in older patients. In younger patients, lumbar facet pain may be the result of an injury. This may occur after a fall or an automobile accident.
How is an endoscopic lumbar EDNA (or rhizotomy) performed?
Endoscopic lumbar EDNA (or rhizotomy) is performed utilizing an endoscope. An endoscope is a small tube inserted into the body, allowing the surgeon to look inside the spine. Because the endoscope is small, only a small band-aid like incision is required. The endoscope has a precision lens on one end and a high definition (HD) camera on the other end. Microscopic instruments are passed through the endoscope to perform surgery. The surgeon visualizes the entire operation, from inside the spine, using the endoscope mounted HD camera. The surgical video is projected on a high-resolution monitor or heads up display.
To start the procedure, a small incision is made on the skin at the lower back, over the facet joint and a few centimeters from the middle of the back. A small tube 7mm in diameter, (less than half the size of a dime), is then placed through the small incision and is advanced to the surface of the vertebra where the pain sensing nerve of the facet joint lies. This nerve is called the “medial branch” of the posterior ramus. A small endoscope is placed through the 7mm tube. Specialized micro-instruments are then used to interrupt (cut) the pain sensing nerve, resulting in a back pain cure. Since the major function of the medial branch is to sense facet joint pain, there are no untoward side effects. Surgery is guided by real time HD video and x-rays.
What are the advantages of endoscopic lumbar EDNA (or rhizotomy)?
Endoscopic lumbar EDNA (or rhizotomy) allows the surgeon to cure pain arising from an injured or painful lumbar facet joint. This allows restoration of normal movement, standing and walking without pain. The tiny opening required for surgery means that there is minimal disruption to the muscles of the low back. The facet joints and ligaments of the spine are untouched, allowing normal stability and strength. Performing surgery through a tiny skin incision and leaving healthy tissues intact means a same day procedure with a quicker recovery.
Probably the most significant advantage to endoscopic lumbar EDNA (or rhizotomy) is that it provides a long-term cure option for patients with lumbar facet pain. Patients can expect a permanent cure from facet joint pain after endoscopic lumbar EDNA. In contrast, commonly performed rhizotomy procedures result in a return of pain in half of all cases by 6 months.
What are the alternatives to lumbar endoscopic lumbar EDNA (or rhizotomy)?
The first-line therapy for lumbar facet pain is facet joint injection. In this procedure, a physician uses x-rays to guide a small needle into the actual facet joint. A combination of anesthetic medications and anti-inflammatory steroid medications are then injected. The main disadvantage of this procedure is that it usually does not last longer than 12 weeks.
Another common alternative is lumbar medial branch block. In this procedure, the doctor uses x-ray guidance to place a needle in the exact location along the vertebra where pain sensing medial branch nerves are located. These nerves sense pain from the facet joint and transmit that information to the spine. From there, the painful stimulus is transmitted to the brain. This is not a treatment. This is performed to diagnose the facet joint as a cause of the patient's pain.
Once the facet joint has been diagnosed as a cause of the patient's pain, the most common procedure undertaken for lumbar facet pain is lumbar rhizotomy. In this procedure, a needle is placed next to the lumbar medial branch nerve which courses along the vertebra. An electrode is placed into the needle. The electrode is connected to a radiofrequency energy generator. The radiofrequency energy results in the generation of intense heat located precisely around the electrode tip. This causes coagulation, or burning, of the medial branch nerve. This results in a loss of painful sensation. The main disadvantage of this procedure is that there is nerve regeneration. As a result, there is return of pain in 6 months in about half of all cases.
How long will the procedure take?
The endoscopic lumbar EDNA (or rhizotomy) surgery typically takes an hour. You will be in the operating room for an additional hour preparing for surgery and preparing for recovery. After the procedure you will recover for about two hours before going home.
What is the recovery like?
After endoscopic lumbar EDNA (or rhizotomy) you go home the same day with pain medications. In most cases light activity can be resumed the next day. Activity should be tolerably increased over 7 days and should consist of short walks, light exercise and a gradual return to normal daily activities. Avoid strenuous activity and heavy lifting (over 10 to 15 pounds) for the first several weeks. If one’s job is sedentary then work can be resumed in 7 days. Recovery time will vary based on individual factors.
Testimonials
Anonymous
The guy really knows his stuff - after reviewing my imaging, we discussed possible procedures. I have done a lot of research online, and had a lot of questions. Dr. Rappard explained the different options, reviewed the pros and cons and offered me a really competitive price. Much better than flying to Arizona for some laser procedure!!
Jacob G.
I am 6 months removed from a couple of branch blocks and then 2 follow up neck procedures. I feel fine, everything is working perfectly. I was willing to accept that Dr. Rappard was a credible, and honest person from meeting with him, and thankfully I can confirm that he is a great doctor, that I recommend to anyone. To be honest, I thought the operating experience was surreal, and I was comfortable. There was a great team, that do their jobs very well, from the anesthesiologist, to the nurse.
Shari A
You saved me from a life of opiates and/or pain so strong that I couldn't perform adequately in my daily activities. After this Rhizotomy procedure, I walked off the table, and except for not drinking the chardonnay, ate dinner with my family. The anesthesiologist, Dr. Paul Rodrick was excellent as well.
Anonymous Patient
I was in a car accident and my lawyer set me up with Dr. Rappard. He is a real straight shooter who wants the best for his patients. He took care of me and totally fixed my back problem. I would highly recommend him.
Anonymous Patient
Dr. George Rappard was very professional and I felt he sincerely cared about my well being. I was injured in a slip and fall and my treatment lasted almost 3 years. I never felt rushed while in his office and received a high level of care. Dr. Rappard kept me appraised of my progress and my experience with his treatment was positive. He did an excellent job with my spinal cord stimulator implant and discectomy. I was very nervous but Dr. Rappard was reassuring. It takes a lot to allow someone to work in your spine, and it is scary, but I trusted Dr. Rappard and he didn't let me down. His office staff are caring, friendly, and terrific! I highly recommend him.
Minimalistic Operations Available for Common Spinal Conditions Don't Wait. Relief Starts Now!
Surgeries
- Advanced Spine Surgery
- Alternatives to Disc Replacement
- Alternatives to Spinal Fusion
- Back Stimulator Implant
- Bulging Disc Surgery
- Bulging Disc Treatment
- Cervical Artificial Disc Surgery
- Cervical Discectomy
- Cervical Microdiscectomy
- Cervical (Neck)
- Discectomy
- Disc Herniation Surgery Los Angeles
- Dr. George Rappard - Cervical Facet Joint Surgery
- Dr. George Rappard-Interspinous Spacers
- Endoscopic Discectomy
- Foraminotomy
- Implanted Spinal Cord Stimulator
- Interspinous Devices
- Laminectomy
- Laser discectomy
- Laser Spine Discectomy
- Laser Spine Surgery
- Lumbar Discectomy
- Lumbar (Lower Back)
- Minimally Invasive Decompression
- Minimally Invasive Herniated Disc Surgery
- Minimally Invasive Neck Surgery
- Minimally Invasive Spine Surgery
- Orthopaedic Spine Surgery
- Percutaneous Discectomy
- Percutaneous Lumbar Discectomy
- Rhizotomy
- Rhizotomy Procedure
- Rhizotomy Surgery
- Sacroiliac (Pelvic)
- Sciatica Surgery
- Spinal Cord Stimulation
- Spinal Cord Stimulator
- Spinal Cord Stimulator Implant
- Spinal Sparcers
- Spinal Spacers for Stenosis
- Spinal Surgery
- Thoracic (Upper Back)